Cats occasionally get plague from infected prey. Eddy Van 3000
The mention of bubonic plague still sends shivers down the spines of people in much of the world. The disease ravaged Asia and Europe for at least 1,500 years, until the advent of antibiotics in the mid-20th century. Many people today believe that plague has been eradicated, and are surprised to learn that the disease continues to thrive in much of the world, though in a rather different form from in its heyday.
Plague is but a shadow of its former self, but it refuses to go away completely. The United States and Madagascar, two reservoirs of the Yersinia pestis bacteria that cause plague, continue to suffer regular outbreaks of the disease. While this scourge may well continue to decline to very low levels, its eradication will be all but impossible unless we understand better where these bacteria like to hide in between outbreaks.
A Tainted Past
The WHO reports 21,725 cases of plague during the first decade of this century, with 1,612 deaths. While isolated cases of the disease can emerge in many places, a handful of plague cases tend to appear each year in Madagascar, the Democratic Republic of Congo and a contiguous area of NW Uganda, Tanzania, Peru, and the United States. Madagascar is by far the hardest hit, with annual outbreaks affecting hundreds of people.
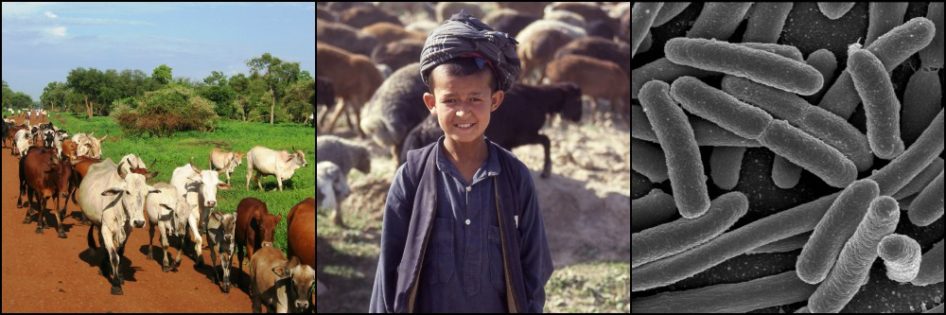
Yersinia pestis bacteria dwell in various rodent species hosts and are transmitted to new hosts by fleas. Periodically large numbers of rodents die off in a given area and the fleas living on them are forced to find new hosts. When rodents are few, the fleas are not averse to settling on nearby people and their pets, to which they may transmit the plague bacteria through their bites.
Once a person is infected through a flea bite, the bacteria migrate quickly to the nearest lymph node, where they multiply and cause significant lymph node enlargement. These visible swellings have been called buboes, whence the name bubonic plague.

The classic bubo, or enlarged lymph node, of a bubonic plague victim. CDC
Two other forms of the disease include pneumonic plague, resulting from either inhalation or spread of the bacteria from the lymph nodes, and septicemic plague, resulting either directly from a flea bite or from spread from lymph nodes or the lungs into the bloodstream. In later stages, the disease provokes coagulopathies (abnormalities in the blood’s ability to clot). Subsequent black bruises on the victim’s body explain the other nickname of “black death.”

Blood clotting abnormalities in some plague victims result in severe bruising and necrosis. The name of “black death” stems from this. Public Health Images Library
Prior to the use of antibiotics in the early 1940s, over 2/3 of plague victims died from the disease. This has declined to less than 13% today, but antibiotics require administration very early in the disease process to be effective.
Life Cycle Peculiarities
Historically, and still in many parts of the world, plague tends to be associated with poor sanitation infrastructures, allowing rats and other rodents potentially harboring Y. pestis, along with their fleas, to live in close proximity to people.
In the US, the bacteria arrived at various ports through the 19th century, but failed to establish themselves permanently until 1894 in San Francisco. Within a decade and a half, Y. pestis spread from urban rats and fleas to rural ground squirrels nearby, and over the next 40 years to rodents in much of the western half of the country.
While urban cycles of disease no longer exist in the US, in some parts of the country plague is becoming a phenomenon of suburban developments in semi-arid regions, such as New Mexico. Nonetheless rural communities are also affected, and the western US comprises one of the more geographically widespread reservoirs of plague in the world. Many cases result from outdoor activities that expose people and their pets to rodent reservoirs (and their fleas), including various species of squirrels and chipmunks, deer mice, wood rats, prairie dogs, and voles. New Mexico, Arizona, Colorado, and California are the most common states for plague cases.
Domestic cats are highly susceptible to Y. pestis, whether from flea bites or consuming infected prey. They develop draining abscesses that can be spread to their owners or, more likely, to their unsuspecting veterinarian who examines the cat without adequate precautions. Transmission to people can result from a bite or scratch, or from inhaling respiratory droplets from an infected cat. Dogs, on the other hand, rarely show serious clinical signs or develop enough bacteria in their bloodstream to infect either people or fleas.
The Role of the Flea
At least 80 of the world’s 2,500 or so described species of flea can be infected with Y. pestis. However, many of these, including the common cat and dog fleas, can carry only small amounts of the bacteria and are not efficient vectors. In addition, individual fleas tend to feed on the same individual animal host during the insects’ short lifespan of a few weeks to months, limiting spread to other hosts.
Some of the more efficient flea vectors, in particular various Xenopsylla spp., undergo a peculiar process that facilitates plague transmission. After taking a blood meal from an infected mammal, Y. pestis bacteria multiply and form a large clot in the flea’s upper GI tract. During subsequent feeding, this clot blocks ingested blood from advancing to the midgut for digestion. The starved flea increases its feeding attempts and in the process tries to expel its bacterial clot. It is unsuccessful, but in the process smaller clumps of bacteria are regurgitated onto the host, leading to infection.

A male Oriental rat flea (Xenopsylla cheopis), engorged with a blood meal. This species is a a primary vector of plague between rodents and from rodents to people. Wikipedia
Problems with this Scenario
This picture of how plague spreads contains some important gaps, however. One question is where the plague bacteria hide in between outbreaks. Nearly all the rodent species that may play a role in plague transmission die rapidly from the disease. To infect a flea, a mammal must have very high levels of Y. pestis bacteria in its bloodstream (probably at least 106 colony forming units per ml of blood). Most rodents cannot support such heavy bacterial loads for more than a day or two at the most before dying. So the number of fleas they can infect is limited to this short time period, believed by many to be insufficient to spread the disease effectively.
When rodent populations are high, for example following abundant rains that increase vegetation for the rodents to feed on, the flea population increases in tandem. When the abundant food declines to normal levels, the dense rodent populations die back and their fleas move to a new host, spreading plague in their wake and spilling over into cats and sometimes people.
Researchers seem comfortable with this “outbreak” scenario. But during non-outbreak periods, rodents and their fleas do not appear numerous enough or dense enough in most plague areas even to maintain the bacteria at low levels. So why doesn’t the plague die out?
Hide-and-Seek
Several ideas have been proposed. One is that Y. pestis may survive in the soil around infected carcasses for long periods between outbreaks, eventually infecting a passing host to keep plague alive. But, while the bacteria can survive for weeks in a carcass, they appear prone to rapid desiccation in the soil.
Others propose that some flea species may harbor the bacteria for many months, even up to a year, preserving it between outbreaks. But why this flea doesn’t transmit the disease to its rodent host and kill it, and why it can suddenly start to transmit the disease to other hosts and spark an outbreak, are not easily explained.
Another idea is that some unknown animal species that is relatively resistant to plague acts as a reservoir for the bacteria. Perhaps more likely is that within a population of a known rodent host species, certain individuals are more resistant to plague than others and are able to carry the bacteria for weeks to months with few or no ill effects. Indeed, this is what happened to some degree in the human population prior to antibiotics, in the small proportion of victims who survived a bout of the disease.

World distribution of plague, 1998, from Centers for Disease Control. The situation is largely the same today. Wikimedia Commons
Answers from Madagascar?
Plague epidemiology in Madagascar is complex, but may hold some answers for how Y. pestis persists in other parts of the world. Three distinct outbreak cycles are present on this island nation, one in rural highland areas, one in forests, and another in urban centers, each with different mammalian hosts, flea vectors, and seasonal patterns.
Similar to the US, plague arrived in Madagascar by boat in the late 19th century from Asia. It spread slowly to the interior highlands over the coming two decades, causing outbreaks there as disease incidence declined in coastal towns. The island has reported over 20,000 human plague cases since 1957, and today still accounts for around 1/3 of plague cases worldwide.
In Madagascar, the black rat (Rattus rattus) is ubiquitous in both rural and urban areas. It likely played a major role in the re-appearance of urban plague cases in Madagascar’s capital beginning in 1979, after an absence of nearly 60 years. But by the 1990s, the black rat had been replaced as the dominant rat species in the city by the brown rat (R. norvegicus), which thrived in the capital’s new sewer networks and modern buildings.
The habits of the brown rat bring it into less frequent contact with people than the black rat. In addition, the brown rat has developed some resistance to the plague bacteria, allowing a larger number of individuals to survive infection than for most other host species. As a result, the city rats avoid large die-offs when plague runs rampant, allowing fleas to remain on the rats rather than have to find new, sometimes human, hosts when their rat host dies.
This scenario, however, presents a double-edged sword. Resistant rats and their fleas may less commonly transmit plague to people, but the conditions seem perfect for a constant, low level of plague circulation in the affected cities that is virtually impossible to eliminate.
Resistant rats, in this case black rats, have also been found in rural areas affected by plague (but not in plague-free areas!). During the rice harvest season, these rats move from human houses to the fields, where the abundant food source leads to high reproductive rates and growing rat, and flea, populations. Plague transmission is low because the fleas have plenty of rat hosts to feed on. With the harvest over, food sources decline and cold weather slows rat reproduction. Surplus rats die and the fleas jump ship in search of other hosts. That is the beginning of plague season in Madagascar’s highlands.
Curiously, outside of the plague season, Y. pestis has not been isolated from rodents, fleas, or any other animals in rural Madagascar’s endemic areas. So in many ways we are right back where we started in trying to identify a key reservoir host for plague. But resistant rodents such as rats undoubtedly play a role.
Resistant Reservoirs
Resistance to plague in rodent hosts is not unprecedented. On the steppes and mountains of Central Asia, the presumed cradle of plague, great gerbils (Rhombomys opimus) and marmots (Marmota spp.), respectively, each harbor a significant number of individuals resistant to plague (as many as 60% in the case of great gerbils). As described in an earlier post regarding West Nile Virus and Zikavirus in the Americas, these Central Asian hosts have evolved with the plague bacteria and its ancestors for thousands of years.
American mammals have had only a century or less to evolve defenses against the disease. But it is possible that in the US too a resistant host or, more likely, resistant individuals within a host species population, have evolved to act as long-term reservoirs for the low-level maintenance of plague in affected areas. Little work has been done, but some studies propose deer mice (Peromyscus maniculatus) and California voles (Microtus californicus) as good candidates.
Elimination of rats in Madagascar, or of similar rodent hosts of Y. pestis in the rest of the world, is unrealistic at best. But a better understanding of where the plague bacteria survive when not causing an outbreak can help us better focus our efforts. These may include population control of key host species and public awareness of the risks to people and their pets in interacting with them, as well as risks posed by increasing expansion of humans into undeveloped areas where plague reservoirs and vectors may be present or accidentally introduced.
References
Andrianaivoarimanana V. Kreppel K, et al. Understanding the Persistence of Plague Foci in Madagascar. PLOS Neglected Tropical Diseases. 2013 Nov; 7(11): 1-8.
Eisen RJ and Gage KL. Adaptive strategies of Yersinia pestis to persist during inter-epizootic and epizootic periods. Vet Res. 2009 Mar-Apr; 40(2):01.
Gage KL and Kosoy MY. Natural History of Plague: Perspectives from More than a Century of Research. Annu. Rev. Entomol. 2005; 50: 505-28.
Kugeler KJ, Staples E. et al. Epidemiology of Human Plague in the United States, 1900–2012. Emerg Infect Dis. 2015 Jan; 21(1): 16-22.