
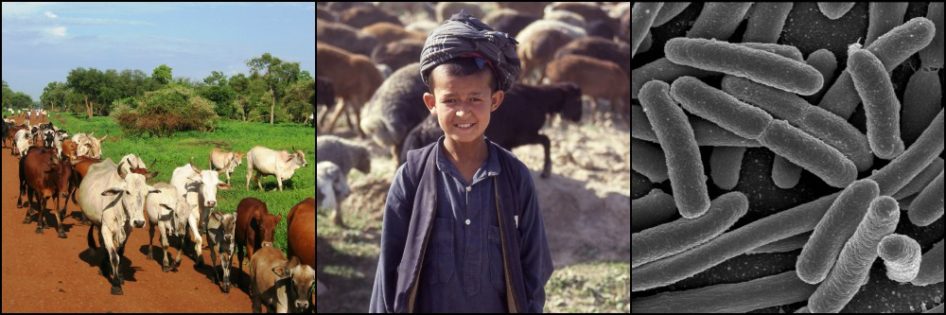
Water-logged soils in the monsoon season make carcass burial problematic in Bangladesh Wikimedia
The month of May 2016 has seen over 100 human anthrax cases in Bangladesh, the seventh such outbreak in the past eight years. The Bacillus anthracis bacteria that cause anthrax began wreaking havoc in Bangladesh beginning in 2009, reportedly a quarter century after the last known human case of the disease in the country.
Anthrax remains a problem not just in tropical climates. It can occur from Sweden to Australia, and from the United States to southern and eastern Europe, and beyond. Research sparked by the 2001 anthrax letters used as a bioterrorist agent in the US filled many gaps in our knowledge. Yet questions about the recent Bangladeshi outbreaks reinforce how much more there is to learn about this often deadly disease.
A Peculiar Life Cycle
Bacillus anthracis infects a wide variety of mammals and some birds. Grazing herbivores such as cattle and sheep are the most commonly affected, and humans are secondarily infected through exposure to these.
The bacteria exist in two forms. One is the vegetative state that exists inside a susceptible animal, in which metabolism and multiplication proceed as is popularly envisioned for “normal” bacteria. But this vegetative form is rare. B. anthracis spend the vast majority of their time as dormant spores.
In a susceptible animal, the vegetative bacteria produce toxins, killing the animal in anywhere from 1 to 14 days. One toxin causes necrosis of vessel walls and the blood of anthrax victims commonly fails to coagulate properly after death, resulting in blood flowing from the orifices and contaminating the area.
On exposure to the carbon dioxide in air, the bacteria produce spores, containing an outer covering highly resistant to sunlight, desiccation, high temperatures, and many disinfectants. Spores can lie in wait for decades, by some accounts even a century or two, to be ingested by another animal and emerge from their deep sleep, starting the cycle again.

Bacillus anthracis life cycle, showing the two forms of the bacterium CDC
The onset of anthrax in infected animals is often so rapid that no signs of illness are noticeable prior to death. “Lightning strike” is cited by textbooks as one rule-out diagnosis when anthrax is suspected. In other cases, cattle may show a fever and irritability, followed by depression and usually death within a day or two.
Anthrax in people can be via consumption of contaminated meat (gastro-intestinal anthrax), through inhalation of spores, or through contact of open wounds with spores (cutaneous anthrax). The latter two are common through butchering of carcasses or processing contaminated skins or wool.

An eschar, the hallmark of cutaneous anthrax, on the neck of a patient. The black color led the ancient Greeks to call the disease anthrakis, meaning “coal.” CDC
B. anthracis has changed little over the millennia. With so much time spent as dormant spores, the number of new generations produced is very low. This limits the opportunities for genetic mutations that drive changes. But the pathogen is so effective at biding its time, spreading from one host to another when opportunities are optimal, that there seems little to improve upon.
The Bangladesh Outbreaks
Human anthrax since 2009 in Bangladesh has been limited to the cutaneous form of the infection, including the more than 600 anthrax cases in 2010. Miraculously, timely treatment prevented any known deaths from the disease. All but a handful of the cases could be traced to slaughtering sick animals or handling contaminated raw meat.
Weather
Bangladesh appears in many ways well suited to anthrax. In general, the disease is popularly believed to occur in the aftermath of unusually heavy rains. In the case of Bangladesh, this is true (though in other parts of the world anthrax can occur in different scenarios, including drought). The recent outbreaks have all occurred during the monsoon season, which lasts from May to November.
B. anthracis spores are ubiquitous but sparse in nature, and low doses are not enough to cause disease. Hundreds of thousands to millions of spores are needed to cause disease in most healthy animals. The rain hypothesis proposes that floods pick up B. anthracis spores in the soil and collect them in low-lying areas. As these pools dry out, heavy concentrations of spores are deposited on vegetation, from which they are ingested by grazing livestock in high enough quantities to cause disease. Biting fly populations also increase in the rainy season, and these are known to contribute to the spread of anthrax in some instances.

The principal anthrax outbreak areas (see map above) are located in the crook above where the Rivers Ganges and Brahmaputra merge. Geography-Bangladesh
Feed
B. anthracis spores are commonly found in the bones left behind by infected animals. Bangladesh imports bone meal, made from ground up animal bones, to feed to livestock, a practice that has been forbidden in many parts of the world to help prevent bovine spongiform encephalopathy (aka mad cow disease, see earlier post). When contaminated bones are included in the mix, anthrax outbreaks can occur. And contaminated forage collected locally can also be a source of spores to infect livestock.
Lack of Vaccines
Animal healthcare in remote areas of Bangladesh is rare. And the anthrax vaccine is only protective for 6-9 months in animals, so regular boosters are needed to maintain immunity in anthrax-prone areas. And for an estimated 49 million ruminants in Bangladesh, the country’s two vaccine laboratories reportedly produced around 4 million doses each year through 2010. All of this militates against effective control of anthrax through vaccination.
Poverty and Public Awareness
In areas most prone to anthrax outbreaks in Bangladesh, the typical family owns a handful of cattle and one or two goats. Cattle are housed beside the home and goats are often kept inside the home at night. Poverty is deep-rooted and families can little afford to lose such a precious resource as a cow or even a goat.
If the vegetative B. anthracis are prevented from exiting their victim after death, the bacteria will die after 2 to 3 days without forming spores. This requires that the carcass remain intact and the orifices are plugged to prevent leakage of blood onto the ground.
But public awareness of anthrax is poor (and not only in Bangladesh). More commonly, when an animal falls seriously ill, the owner will slaughter it before it dies. The animal is butchered and the meat eaten by the family or sold. The carcass is skinned and the hide sold in the leather market. Different and often numerous people perform these various tasks, exposing themselves to any eventual spores.
Inappropriate Carcass Disposal
Subsequent abandonment of the carcass in fields or water courses leads to further exposures. But even if villagers knew to burn and bury carcasses to prevent further transmission, fuel for burning is scarce and expensive, and burial in the water-logged soils of the monsoon season is problematic.
Previously, wildlife and much livestock that died of anthrax were cleaned to the bone by vultures so quickly that spore formation could not occur. But vulture populations have been decimated, thought to be due to the continued, widespread, illegal use of diclofenac sodium that kills vultures scavenging on livestock treated with this non-steroidal anti-inflammatory drug. Without the vultures, other scavengers spread animal parts far and wide, trailing spores along the way.
Outbreak Enigmas
Despite many of the “classic” characteristics of Bangladesh’s recent anthrax outbreaks, several mysteries remain. One is their tendency to erupt at the height of the monsoon season, which would not be expected even in the heavy rain hypothesis described above. During these months of heavy, regular rains, pools don’t have time to dry out, thereby preventing the concentration of spores on surrounding vegetation. This usually occurs only during the early dry season.

Monsoon clouds over Bangladesh, photographed from the International Space Station NASA
Furthermore, it was reported in one recent paper that multiple strains of B. anthracis, some not found before in Bangladesh, were identified from the 2010 anthrax outbreak. The suggestion is that imported bone meal contaminated with spores may be the culprit. Yet affected villagers deny feeding bone meal to their animals. And even if contaminated feed were involved, anthrax cases would likely be distributed more evenly throughout the year.
Most worrying is the unexplained emergence of widespread and regular outbreaks beginning in 2009. Anthrax can be difficult to diagnose and cases may have gone unnoticed over the preceding years. But in general the disease appears not to have been a major problem before. And the cyclical appearance of outbreaks during the monsoon season in seven of the past eight years is highly unusual. Even in endemic countries, the timing of anthrax outbreaks tends to be unpredictable. What has changed?
Widespread consumption of contaminated meat has also been a feature of these outbreaks, yet reportedly no cases of gastro-intestinal anthrax have been diagnosed. Many victims of the cutaneous form may have also suffered from GI anthrax and were treated successfully for both with antimicrobials. But under the circumstances, at least some GI cases would have been expected.
Bringing Anthrax Under Control in Bangladesh
The solutions to preventing the annual emergence of anthrax outbreaks in Bangladesh are no secret, least of all to Bangladeshi authorities. But, for reasons already noted, implementation is not a simple matter. A concerted vaccination campaign with timely boosters in high risk areas is the surest way to limit anthrax in livestock. And preventing anthrax in livestock prevents anthrax in people. But getting enough vaccines to remote, high-risk areas has so far proved difficult, despite some efforts.
Public awareness is critical to catching and treating disease early. But even those aware of appropriate carcass disposal have limited options during the floods of the rainy season. Risks will still be taken to salvage the meat and hides of severely ill animals. Closing off grazing lands that may be contaminated with B. anthracis spores is also not an option in this densely populated country, particularly during the rainy season when dry land is limited.
Despite these handicaps, Bangladesh has somehow managed to keep human deaths from recent anthrax outbreaks to a minimum, or even non-existent if all cases have been diagnosed. While recent patterns of the disease in Bangladesh can largely be explained, remaining mysteries remind us that we still have much to learn about this ancient disease.
References
Fasanella A, Garofolo G, et al. Bangladesh anthrax outbreaks are probably caused by contaminated livestock feed. Epidemiology and Infection. 2012; 141(5): 1-8.
Saiful Islam Md, Jahangir Hossain M, et al. Risk practices for animal and human anthrax in Bangladesh: an exploratory study. Infect Ecol Epidemiol. 2013; 3.
Shaheenur Islam SK, Castellan DM, et al. Animal anthrax in Sirajganj district of Bangladesh from 2010 to 2012. Asian Journal of Medical and Biological Research. 2015; 1(3):387-395.
World Health Organisation (2008). Anthrax in Humans and Animals (4th ed.). Geneva: WHO.





Hi Dr. Hoots!
This was a very interesting post. I was wondering how, when an animal gets infected, the rest of the herd is handled? Are they assumed to be exposed and potentially infected and have to be slaughtered or do the owners typically wait to see if they exhibits signs of infection? I know you mentioned that owners typically don’t have many animals so I imagine they are loathe to slaughter seemingly unaffected animals preemptively.
Also, you mentioned that the vaccine is only effective for a short time period. Any idea why that might be?
Finally, as my background is in genetics, I was very interested in your comment that there’s little to improve upon in terms of fitness (certainly looks that way!). Do you know if the genome is sequenced and if so whether there appears to be any potential for using genetic engineering to combat Anthrax? I suppose given its relatively low impact on humans (in terms of number of deaths) there might not be sufficient funding for that sort of thing.
Again, very interesting and informative post!
Hi, Alexis. Thank you for your comments!
You are correct that slaughtering the rest of the herd is not an option for most. Nor is it necessary as anthrax, with possibly some rare exceptions, is not considered contagious between live animals or people (so long as there is no bleeding).
Identification and elimination of the source is important. Antibiotics can be given to animals known to be exposed, and vaccination for those at lower risk. But both in the same animal at the same time is not advised because the animal vaccine (but not the human one) is comprised of modified live bacteria. The antibiotic may kill the bacteria in the vaccine before they can multiply and produce an immune response in the animal.
The most commonly used anthrax vaccine for animals was developed by Max Sterne in South Africa in 1935. He used bacterial attenuation techniques developed earlier by Louis Pasteur for his own anthrax vaccine, but which caused unacceptably high numbers of death in vaccinated animals. Very little seems to have been done to look at the length of immunity in vaccinated animals. It is stated simply that protection is “likely” to last at least 6-9 months, and maybe up to a year. The human vaccine is even more onerous, requiring five initial doses over 18 months, then annual boosters.
I hesitated to include the very subjective comment that there is “little for the bacteria to improve upon.” As a geneticist, I’m glad you didn’t take offense (or maybe you are just diplomatic!). I wonder if anthrax simply kills so few animals and people that there is little or no selection pressure on these hosts to evolve resistance to it. In which case nor would the bacteria be pressured to change much.
The funding for studies on anthrax in humans I think received a big boost in the aftermath of the 2001 anthrax letters. The entire genomes of several strains have been sequenced (see Bacillus anthracis: Molecular taxonomy, population genetics, phylogeny and patho-evolution). The first, I believe, was in 2003. Early on there was speculation that this would lead to new vaccines or antimicrobials. But I haven’t seen many developments along these lines since. While the vaccines (both animal and human) can certainly be improved upon, penicillin, fluoroquinolones, and/or tetracyclines already work quite well against anthrax, provided it is caught early enough.
Hi Dr. Hoots,
Has anthrax ever threatened wildlife populations? If so, has it ever led to major population declines? Thank you in advance for your time.
Yes, Stephanie, anthrax can pose a problem for wildlife around the world. Sometimes hundreds of animals perish in a single outbreak, but impacts on whole populations depend on many factors, most importantly the size of the original population, but also differences in susceptibilities according to sex and age of individuals, among others.
Anthrax in South Africa’s Kruger National Park reportedly wiped out half of the park’s roan antelope population in 2012. Impala antelope can also suffer heavy losses to anthrax, but their absolute numbers are much greater than the roans’ and so the impact is less severe.
The same goes for hippos, whose habit of communal feeding on carcasses makes them especially vulnerable to anthrax. The first, and only, anthrax I have seen was under a microscope at a veterinary lab in Uganda, taken from a deceased hippo in Queen Elizabeth National Park in 2009. Over 80 hippos reportedly died from the disease in the park the following year. Zambia and Zimbabwe also suffer hippo losses from anthrax.
Among bison in North America, and wildebeests and elephants in Africa, young males are much more likely to contract anthrax, and sometimes large numbers perish. But because they are limited to mainly males, overall population levels of these species are not overly impacted.
Botzler and Brown’s book “Foundations of Wildlife Diseases” has a good section on anthrax. They have an interesting discussion of shifts in anthrax epidemiology in relation to man-made ecological changes.
Though a bit dated, online you can take a look at the OIE paper by Hugh-Jones and de Vos, “Anthrax and Wildlife” at
http://www.oie.int/doc/ged/D520.PDF.
And keep an eye out for a future post on this subject. It is an interesting one!
Am a Zambia,am a veterinary laboratory diagnostics officer in the civil service,going by reports of anthrax which had heat the western province party of Zambia I wish to ask is there any chance of it resurfacing?
Hello, Martin.
Unfortunately there is every chance that anthrax will resurface in Western Province. It seems to do so almost every year. As eliminating the anthrax spores in the ground is impossible, prevention through vaccination of livestock is of critical importance. In addition, public awareness of how to suspect anthrax in a sick or dead animal, including wildlife, is also important, to prevent consumption of the meat. Is it possible for large numbers of herders in that area to vaccinate their animals?