Construction of the Panama Canal spurred research to develop a yellow fever vaccine Library of Congress
With yellow fever vaccine in short supply in the face of an ongoing outbreak in Angola, we might be reminded of the fortuitous, and by no means inevitable, circumstances that led to the development of the yellow fever vaccine in the first place. Vaccines for mosquito-borne diseases are hard to come by, and no less so for the flaviviruses that include yellow fever, dengue, West Nile, and Zika viruses. A serendipitous event in a yellow fever virus isolated from a single person 90 years ago has given rise to all yellow fever vaccines in use today, though at a heavy cost to many of those who played a role in its discovery.
Yellow fever was the scourge of the Americas and much of Africa in the 19th and early 20th centuries. The great majority of people infected with yellow fever virus suffer no, or very mild, symptoms. A minority however, develop fever, nausea, and muscle pain for about a week, then recover fully and are immune for life. In about 15% of these clinical cases, the disease progresses to internal hemorrhaging and organ failure, particularly of the liver, producing the characteristic jaundice for which the disease is named. One in five of those affected with this severe form of the disease may die.
Construction of the Panama Canal (completed in 1912) was seriously impeded by the number of laborers falling ill to the virus. When it was realized that the canal’s opening would concentrate unprecedented numbers of immunologically naïve people from around the world in an endemic yellow fever region, funding was earmarked to find a solution.
It was demonstrated in 1900 that the Aedes aegypti mosquito transmitted yellow fever virus between people. Measures to control this mosquito species rolled back the disease in many places, but its persistence, particularly in the tropics, suggested there was more to this disease than met the eye.

Yellow fever range in tropical South America and Africa Sanofi Pasteur
Ae. aegypti indeed spread the virus between people in what is now known as the urban yellow fever cycle. But a sylvatic cycle also exists, in which different mosquito species spread the virus between forest-dwelling monkeys.
That would not be a problem for people except that the two cycles are at times linked via an intermediate cycle, in which mosquito species that may feed on both monkeys and humans spread yellow fever virus between the two. On discovery of this complicated epidemiology in 1911, identification and elimination of the numerous mosquito species involved was not feasible and attention was turned to developing a vaccine instead.
Finding a Vaccine Candidate
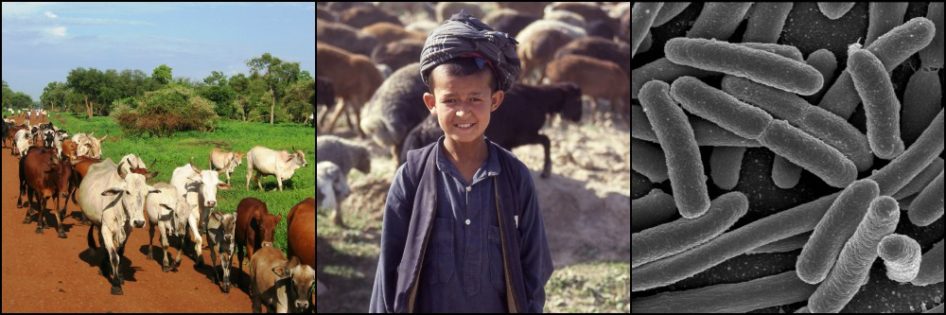
In 1927 yellow fever virus was isolated by researchers from a Mr. Asibi, a 28 year old West African man in what is now Ghana who was suffering from a mild case of the disease. South African researcher Max Theiler was aware of Louis Pasteur’s earlier success in attenuating (reducing the virulence of) rabies virus by repeatedly culturing the virus in one rabbit brain tissue specimen after another. Theiler noticed that, similarly, yellow fever virus became less virulent as it was inoculated into a series of rhesus macaques.

Mr Asibi, the man from whom the first yellow fever virus was isolated, and from which all YF vaccines in use today derive. Rockefeller Foundation
Using this advantage, in 1932 Theiler and his colleagues began growing the Asibi strain of virus in a series of 17 mouse embryos, followed by 58 chicken embryos, then tested it. As they suspected, the effect of the resulting virus on the heart, liver, and kidneys of inoculated rhesus macaques had nearly vanished. Unexpectedly, however the virus’s tendency to cause encephalitis (brain inflammation) not only remained but was increased. The researchers tried injecting lower doses of the virus into the monkeys, but strangely this only increased the frequency of encephalitis in the monkeys.
Next Theiler and his team turned to dissecting out all brain and spinal cord tissue from the chick embryos in which the virus was cultured. They hit the jackpot! After passage through another 100 or so denervated embryos, the researchers found that the virus no longer caused encephalitis in either mice or macaques.
A handful of chance and very fortunate mutations were responsible for these changes. The mutated virus produced few to no side effects and induced a strong immune response in monkeys, effectively protecting them against wild yellow fever infection. This vaccine strain was dubbed 17D (reflecting the initial 17 passages of the virus through mouse embryonic tissues).
Much later, it was found that the 17D virus’s genome differed by only 68 nucleotides out of the 10,860 nucleotides making up the entire viral genome. But it was enough to change everything. Successful testing on human volunteers began in 1937, including on Theiler and his team.
Over the years, yellow fever virus was isolated from many different individuals and passaged hundreds of times through various tissue cultures. Remarkably only the Asibi strain, the very first isolated, eventually produced a mutation sufficiently attenuated to be safe for humans while simultaneously provoking a long-lasting, protective antibody response in vaccinated people.
Hiccups along the Way
In the early days of using the new yellow fever vaccine, occasional outbreaks of liver damage occurred in vaccinated people. During World War II, some 8 million soldiers were vaccinated, of whom 80,000 developed liver disease and 81 died.
An investigation discovered the problem. Small amounts of human serum were included in the vaccine to improve its stability. Serum used in certain vaccine batches had been collected from persons infected with hepatitis b virus, which subsequently infected some of those vaccinated. Serum was determined not to be necessary for the vaccine’s stability and its use was immediately discontinued.
A further hiccup emerged in 1941 when 119 persons vaccinated for yellow fever developed encephalitis. It was found that virus used to formulate more vaccine had been passaged many more times through tissue cultures. It was believed that a further mutation occurred during these passages that caused the virus to affect nervous tissue.
The higher the number of viral “generations” produced from the parent 17D strain, the higher the risk of mutations leading to increased virulence or, in some cases, ineffectiveness in the vaccine virus. To combat this, a mechanism was needed that would prevent parent strains of the 17D virus from being passage cultured ad infinitum to continuously produce new vaccine batches.
This was achieved through the establishment of a library of 17D strain “master seeds.” These master seed viruses alone were to be used in future vaccine production. But only up to a point. Once serially cultured a certain number of times (often about 30 passages), no further vaccine could be produced from these viruses. Additional batches would have to start over again with the same or another master seed virus. Encephalitis cases related to genetic changes in the vaccine virus stopped with implementation of the seed system.

Max Theiler, credited with developing the yellow fever vaccine. Wiki
Success Story
Attenuating viruses, ridding them of contaminants, and producing vaccine on a massive scale was cutting edge work in the 1920s and 30s. The resulting yellow fever vaccine was the first live, attenuated vaccine to see the light since Jenner’s smallpox vaccine nearly a century and a half earlier.
Two 17D virus substrains traced back to Mr. Asibi continue to be used to produce the only two WHO-approved yellow fever vaccines in use today. And the vaccines are still produced essentially the same way they were then – grown in chicken eggs. Over half a billion people have been vaccinated to date, with minimal adverse events.
Max Theiler won the 1951 Nobel Prize, the only recipient awarded for development of a viral vaccine. But the price to the scientific community was heavy. Theiler contracted yellow fever while working in the lab, but suffered only mild illness. At least six of his colleagues were not so lucky, succumbing to the virus while researching it. Today yellow fever continues to infect some 200,000 people and kill over 30,000 each year on average. But without the serendipitous discovery of the vaccine, the toll would undoubtedly be much higher.
References
Frierson JG. The Yellow Fever Vaccine: A History. Yale J Biol Med. 2010 Jun; 83(2): 77–85.
Norrby, E. Yellow fever and Max Theiler: the only Nobel Prize for a virus vaccine. J Exp Med. 2007; 204(12): 2779-2784. Retrieved from
Post PR, Carvalho R, da Silva M, and Galler R. The early use of yellow fever virus strain 17D for vaccine production in Brazil – a review. Mem Inst Oswaldo Cruz. 2001; 96(6): 849-857. Retrieved from
Pulendran B. Learning immunology from the yellow fever vaccine: innate immunity to systems vaccinology. Nat Rev Imm. 2009 Oct; 9:741-747.