Lake Victoria from Entebbe, Uganda, near the forest for which the Zika virus is named. Charles Hoots
With concern of a possible connection between Zika virus and microcephaly in Brazilian babies, researchers are racing to fill in the many blanks about the virus in order to better control it. But predicting the future of Zika virus in the Americas is fraught with difficulties. The behavior of closely related, recently introduced viruses offers clues. But despite similarities, the differences are many and prevent sweeping generalities. Though not reassuring to couples contemplating starting a family right now, it is this uncertainty that makes these viruses so fascinating.
Zika virus was discovered in 1947 in a forest along the shores of Lake Victoria near Entebbe, Uganda. Subsequent testing detected the virus in humans in much of Africa and Asia, but only occasionally did it cause even mild illness. Interest faded until 2007, when Zika virus began spreading swiftly across the Pacific islands, reaching South America by 2014.
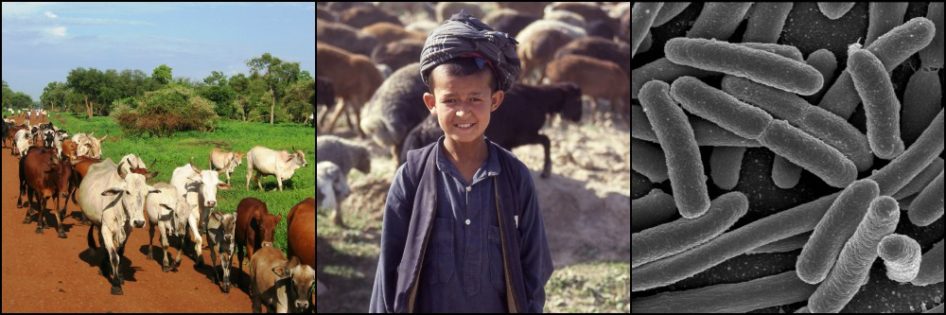
What we know of Zika virus in its traditional range is limited, so understanding it in the Americas is even more difficult. The virus seems to infect humans (and some other primates) with the help of mosquitoes. And there is evidence that various bird species can harbor the virus. It is important to know which of these, and any other, hosts have enough virus circulating in their blood to infect mosquito vectors that feed on them, further spreading the disease.
During its journey across the Pacific, the Zika virus caused more severe illness than previously, with symptoms including fever, rash, and joint pain, the hallmarks of numerous mosquito-borne viruses. Its arrival in Brazil coincided with an unexplained increase in the number of babies born with microcephaly (an abnormally small head). Evidence is mounting that Zika infection during the first six months of pregnancy increases the risk of microcephaly in the fetus, a more worrying scenario than cases of rash and joint pain. But many questions remain.
For one, the recent expansion or introduction of other mosquito-borne viruses (Dengue, Chikungunya) in the Americas have muddied the waters. Is one of these emerging viruses responsible for the microcephaly? Or maybe two or more of the viruses work in concert to cause the birth defect?

Birth defects in lamb born to a ewe who ingested the false hellebore plant during pregnancy. USDA
Understanding the mechanisms of birth defects can be complicated. One of my professors in veterinary school was involved in an investigation in the 1950s into the mysterious case of cyclops lambs in Idaho born with a single eye in the middle of their face. After years of tedious research, it was discovered that the mothers of all of the effected lambs had grazed on a specific plant species, the false hellebore, between days 13 and 15 of pregnancy. Ingestion of the plant at any other time did not cause the defect. This story shows how difficult it can be to link a particular factor to a birth defect.
What can we expect from Zika virus as it spreads through the Americas?
When pathogens are introduced into new areas, they often cause more severe illness than in their traditional range. Smallpox and other diseases brought by Europeans demonstrated this among Native American populations. As discussed in a previous post on avian influenza, a common sign that a pathogen and host have evolved together over many generations is the absence of disease in hosts infected with that pathogen. In new regions, pathogens encounter people and animals with no prior exposure to them, and thus no immune system memory to defend against them.
New environments also result in new relationships with vectors and hosts, some of which may allow the pathogen to spread more effectively than in its traditional range. Over time, the host population builds up immunity and the pathogen tends to cause more moderate disease than early on in the relationship. But much can happen as this process plays out.
Zika virus is a member of the Flaviviridae family, which includes several other viruses present in the Americas. Like Zika, some of these have arrived relatively recently to the New World, making them interesting as potential models for what we can expect from Zika virus.
Dengue virus
This flavivirus is widespread throughout warm, humid areas of the world, where it is spread between humans by the same Aedes mosquito species that are thought to spread Zika virus. Similar to Zika, Dengue virus strains spread across the Pacific Ocean with troop movements during and after World War II. Simultaneous with this expansion, a more severe form of the disease appeared for the first time in humans. This dengue hemorrhagic fever added internal bleeding to the fever, rash, and joint pain found in some infected persons.
The appearance of dengue hemorrhagic fever in Latin America in 1981, popularly called “breakbone fever” due to the intense joint pain, is explained by increased numbers of mosquitoes in urban areas and the recent global spread of the Aedes mosquito species most likely to spread dengue. In addition, dengue virus evolved over the centuries into four slightly different variants, called serotypes. Newly introduced mosquitoes from different regions of the world brought the different serotypes together in a single area. Interactions between them resulted in the more severe form of the disease.
So despite a common trend towards more benign effects of a pathogen on its hosts over time, there can be unforeseen hiccups along the way.
What West Nile Virus Can Tell Us About Zika
This flavivirus has a lot in common with the Zika virus in our story. West Nile Virus (WNV) too was discovered in Uganda (in the country’s West Nile district, birthplace of the infamous Idi Amin) only 10 years before Zika virus. It occasionally causes outbreaks of human illness in its traditional range, but largely keeps under the radar.
WNV was unknown in the Americas until it appeared in New York City in August 1999, killing large numbers of wild birds, smaller numbers of horses, and sickening people on a scale unprecedented in the virus’s normal Old World range. The virus crossed North America within five years, and most of the Caribbean, Central, and South America within a decade. More than 30,000 people in the US have been sick enough from WNV to seek medical treatment and over 1200 have died from it over the decade and a half since it arrived there.
We might be tempted at this point to explain the unprecedented virulence of WNV in North America by the lack of immunity in a naïve population, never before exposed to the virus. And this undoubtedly played a role. But, interestingly, the WNV strain in America appears to have originated from one found in Israel. Similar to the increased illness caused by the Zika virus that arrived in Brazil from the Pacific, the WNV strain in America had begun killing wild and domestic birds in Israel the year before its arrival in America, on a scale never seen in the six decades since the virus’s discovery. So it seems that WNV did not simply arrive in America and cause more severe disease because of the naïve population alone. Rather, a more virulent strain of WNV evolved BEFORE its arrival in America.
Once in the Americas, WNV took on other peculiarities. More than 60 mosquito species are found to harbor the virus in North America alone (though not all of these can transmit the virus under normal conditions). Some of these feed on birds in the summer, then switch to people and other mammals in the fall when birds become scarce, spreading the virus to many different species.

Global map of the predicted distribution of Aedes albopictus. This is a widespread mosquito species suspected of being a major vector for Zika virus. elifesciences.org
Favorable dynamics between the virus and its new mosquito vectors may further explain the spread and virulence of WNV in North America. For example, it typically takes 2 weeks between the time a mosquito vector ingests WNV and the time she can transmit that virus to another blood-meal victim. However, soon after its arrival in the US, a mutated WNV strain appeared in Texas that significantly shortened this 2 week period, allowing more rapid transmission between hosts.
Since its introduction, WNV in the US displays a recognizable pattern. A few, mild human cases are found in the first mosquito season following introduction of the virus to an area. The second mosquito season shows a much larger number of human cases, accompanied by a large number of bird deaths. The third year tends to show many fewer WNV cases in all species, probably due to increased immunity in host populations. Some, but not all, areas thereafter experience periodic outbreaks of WNV influenced by mosquito numbers, increasing populations of unexposed hosts, and undoubtedly many other factors.
Interestingly, compared to North America, WNV has caused much less disease in all species as it spread to Latin America. Some suggest the virus has undergone genetic changes making it less virulent. Another hypothesis is that the prevalence of other Flaviviruses in Latin America (including dengue, yellow fever virus, and others) provides immunity against the related West Nile virus. None of the explanations fully explains this phenomenon to date.
What does all this tell us about Zika Virus?
With all its unknowns, we still know much more about West Nile virus than about Zika virus. We don’t even know yet which animals Zika can infect. It is possible over the next few years that Zika, similar to WNV, will infect enough people and animals (without them even noticing in most cases) that the number of potential new hosts will decline to the point that the virus is maintained at a low, nearly harmless level. This is called herd immunity. Girls will be exposed to the virus before child-bearing age, protecting them from infection during pregnancy and sparing their babies the increased risk of microcephaly (if the two prove to be associated). Even this rosy picture includes occasional local spikes in cases, sparked by any number of factors such as weather patterns promoting increased mosquito populations.
Zika virus may spread to and persist where its eventual mosquito vectors are present, which will likely be a large portion of South and Central America and parts of North America. We can gain some insight into its likely behavior from similar situations with other, related viruses. But making predictions about virus behavior is difficult under the best of circumstances. Until we know more about it, any predictions about Zika virus will be tenuous at best.